Is shared governance the key to unlocking a more engaged and empowered nursing workforce? The evidence suggests that by embracing shared governance models, hospitals and healthcare systems can significantly improve nurse satisfaction, enhance patient outcomes, and foster a culture of collaboration and innovation.
The path to effective shared governance, particularly within nursing units, isn't always straightforward. Challenges can arise, and teams may find themselves struggling to maintain focus and achieve their goals. It's a journey that demands dedication, strategic planning, and a commitment to continuous improvement. But when executed effectively, shared governance can transform a unit, not just in terms of efficiency, but in fostering a work environment that is more collaborative, innovative, and ultimately, more rewarding for nurses.
To further understand the impact and implementation of shared governance, let's delve into the experiences and strategies of a variety of healthcare settings. The insights gleaned from their experiences, whether they involve a community hospital's efforts to increase knowledge or a university hospital's focus on obtaining or retaining a coveted Magnet designation, offer invaluable lessons for any team embarking on this journey.
- Josh Harts Family Background Meet His Parents
- Mark Harmons Date Of Birth Explore The Life And Career Of The Renowned Actor
| Category | Details |
|---|---|
| Name | Shared Governance in Nursing |
| Description | A model of healthcare management that emphasizes collaboration, shared decision-making, and empowerment among nurses. It promotes nurse autonomy and provides nurses with a voice in decisions affecting their practice and work environment. |
| Key Components |
|
| Benefits |
|
| Challenges |
|
| Implementation Steps |
|
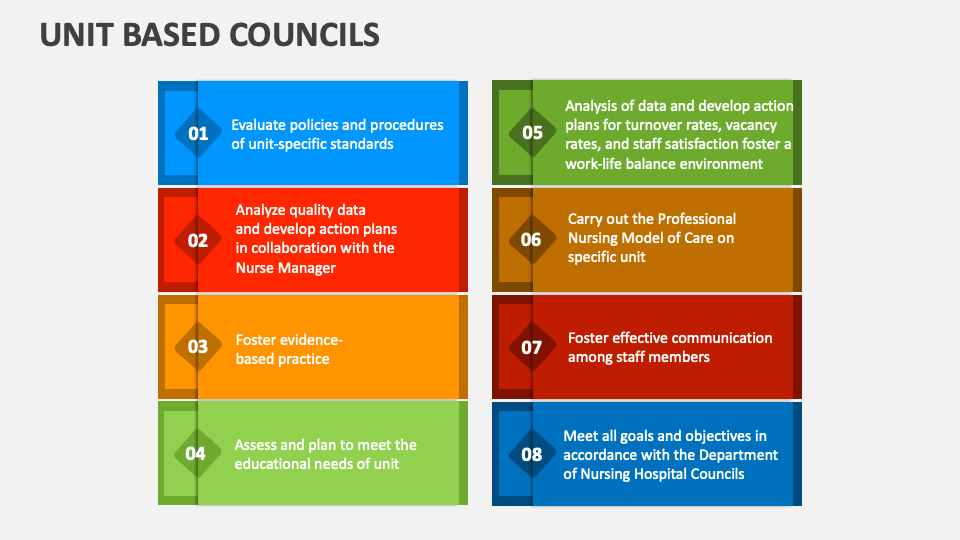
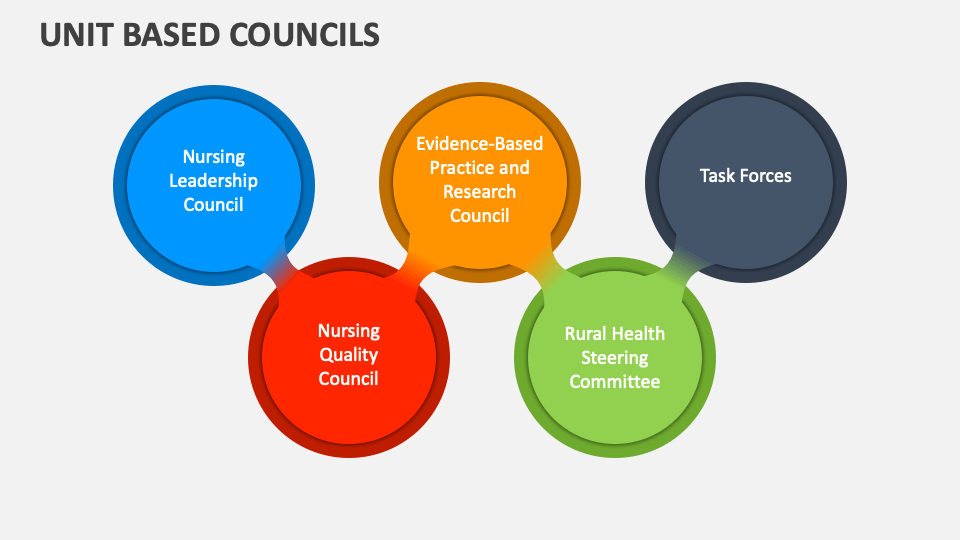
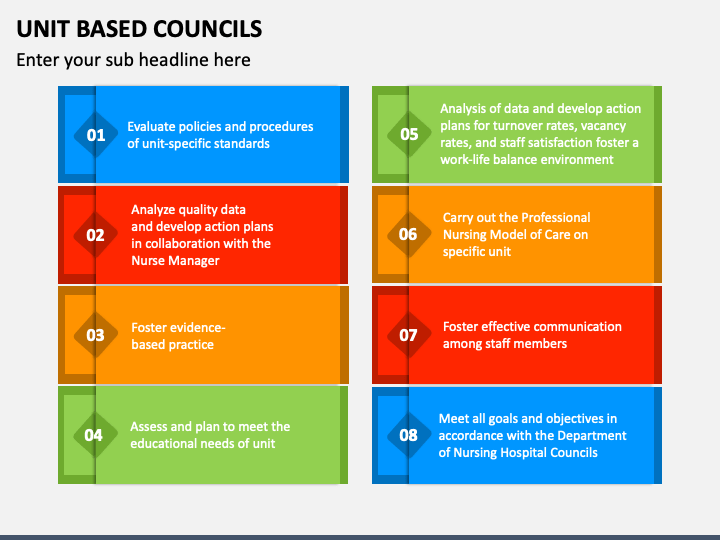
| How it Works | Shared governance operates through various structures such as Unit Practice Councils (UPCs), which serve as forums for nurses to address issues, propose solutions, and participate in decision-making. UPCs can focus on various areas, including clinical practice, quality improvement, staffing, and professional development. |
| Reference | American Nurses Association |
Many specialty organizations publish recommended practices and guidelines, providing a valuable resource for units seeking inspiration and guidance. For those seeking to achieve or retain a Magnet designation, the role of unit-based ideas becomes especially important, as it helps to streamline effective governance.
When a pertinent issue arises, adding it to the meeting agenda ensures the team addresses it directly. The makeup of a unit can significantly affect its functioning. For instance, a unit composed of 45 RNs and 20 HCTs would have different dynamics than a smaller, more specialized team. The level of RN council attendance participation in 2011 and 2012, which was 32% in both years, can provide insights into engagement and the need for initiatives to boost participation. If a unit practice council, which may have gotten off track over time, starts to focus on the right things, it can change the landscape for everyone involved.
Redefining the council's purpose is often the first step toward improvement. As members rotate, it is common for the purpose and focus to become distorted or lost. A skilled leader can get the team back on track by re-establishing clear objectives, outlining actionable steps, and promoting positive attitudes.
Proper training of council chairpersons is important. Orienting them on the basics of planning and running meetings can significantly improve their effectiveness. The CNO of a hospital can also act as a huge advocate for shared governance on the unit level, with a particular focus on quality.
The council's overall structure should encompass how the unit selects its leadership group, how the manager mentors the council in its new authority, and how council members can skillfully discuss issues in a way that promotes resolution. Many unit councils have goals, like developing small, feasible projects to help with night shift workflow. The input and ideas from the broader nursing community, can provide additional context and inspiration for projects, further enhancing the overall scope of the process.
It is worth noting that the leadership team (nurse manager, assistant nurse managers, and unit council staff nurse leaders) plays a key role in making shared governance successful, and nurses must be provided with the necessary skills to succeed. The leadership group also helps in providing direction for the council. Some organizations ask for staff nurse volunteers to participate, while others use elections to determine council members. In either scenario, those involved in the council should be able to give direction regarding the council's core values.
Early and Soeder are advocates of shared governance. They shared ideas with nursing leadership after the meeting and also created meeting minutes. According to Early, shared governance is important and gives nurses a voice with management.
By engaging in shared governance, nurses can develop professionally and gain strong leadership roles. They are given the skills and tools necessary to create positive change, promote interprofessional collaboration, and foster their skills. The author has disclosed no financial relationships related to this topic.
Nurse autonomy is also supported and promoted through this shared governance model. The unit practice council uses a bulletin board to communicate with the unit about council members, current initiatives, new ideas, and ongoing projects. It also holds monthly meetings and produces committee reports.
A community hospital sought to increase knowledge and awareness of shared governance and improve nurse engagement, clinical nurses in that organization demonstrated leadership and innovation by leading specific projects and engaging in system-level councils, thus increasing their voice within the organization. The nurse practice and quality council guides the development, review, and improvement of policies and procedures while evaluating nursing practices using established quality outcome measures.
To ensure that the Unit Practice Council remains effective, its critical to keep it focused on its original purpose. As members change and time passes, goals can become unclear. However, by having a skilled leader, a focus can be re-established and can keep the group on track.
Shared governance models recognize the importance of engaging nurses in decisions that affect their practice. This can lead to improved job satisfaction, reduced turnover, and better patient outcomes. However, simply implementing a shared governance structure isn't enough. It must be properly implemented and continuously evaluated to ensure it is working effectively.
For instance, a unit practice council can address issues specific to a unit, such as workflows, staffing, and patient care protocols. Their efforts can also guide the development, review, and improvement of policies and procedures and also provide an opportunity to evaluate nursing practices using established quality outcome measures. In this way, it's a valuable approach.
Regular evaluations of the council are also important. This can include surveys of nursing staff to gauge satisfaction, feedback from administrators, and an analysis of patient outcomes to determine whether goals are being met. The results should be used to make adjustments and improve the council's processes.
Communication is another cornerstone of effective shared governance. The council should keep the unit informed about its activities, progress, and upcoming plans. This can be done through regular reports, newsletters, bulletin boards, or meetings. This communication helps to ensure that all nurses are aware of the council's work, and it also provides opportunities for feedback and discussion.
Leadership training is critical for council members. These training sessions should cover a wide range of topics, including meeting management, conflict resolution, and decision-making. They can also provide opportunities to discuss challenges and learn how to address them.
Unit practice councils can improve their effectiveness by incorporating these strategies. For instance, the council can establish clear objectives, develop a schedule of activities, and also establish accountability mechanisms. It can also foster a collaborative and respectful environment where all voices are heard and valued.
The journey to shared governance requires commitment, planning, and ongoing evaluation. However, the payoff can be significant for both nurses and patients. By empowering nurses, improving communication, and continuously striving for improvement, healthcare organizations can create a more supportive and effective environment. This collaborative approach can lead to more positive outcomes for nurses and can also transform a nursing unit.
Shared governance models can be adopted in various healthcare settings. For example, a community hospital can increase knowledge and awareness of shared governance and improve nurse engagement. This can lead to better patient outcomes and can also benefit the nurses themselves. Implementing shared governance can be a powerful tool for improving nurse engagement and creating a more positive work environment, but only when it is properly implemented and also continuously evaluated.
In conclusion, shared governance is not just a model of healthcare management. It represents a commitment to creating a more equitable and collaborative environment where nurses can contribute their unique skills and expertise. This process can lead to higher job satisfaction, lower staff turnover, and improved patient outcomes.
- Steve Martins Daughter Meet The Comedians Only Child
- Jonathan Stoddard A Look Into His Wife And Personal Life